Dr. Robert Van Boven, the Whistleblower
Lakeway neurologist battles hospitals, officials, and the "culture of silence"
By Michael King, Fri., April 20, 2018
When Marcus Turner awoke one morning in November of 2014, he noticed numbness in his arms and legs – from his elbows to his fingertips, from his knees through his feet. Turner was a triathlete, in excellent condition, and was alarmed by his inexplicable symptoms. As it happened, a relative visiting at the time was a doctor of physical therapy, and he told Turner, "I can't explain this. There's something seriously wrong."
Turner's wife drove him to the emergency room of the Lakeway Regional Medical Center (near Highway 620). He would spend the next dozen hours, until nearly midnight, being examined by four different doctors – one told him he likely had AIDS, another guessed multiple sclerosis. The fourth doctor to examine him was a neurologist, who after a brief review of the record and a cursory examination told him he was suffering from "stress and anxiety" and should go home and get some rest.
Turner knew better, and insisted – over hospital staff objections – on getting the opinion of another neurologist, Dr. Robert Van Boven, who had been present during some of his earlier tests. Van Boven began what Turner recalls as a thorough interview and physical examination, and eventually concluded that Turner's symptoms indicated Guillain-Barré syndrome, a quickly advancing autoimmune disorder that destroys the nervous system, usually beginning with the extremities, and if left untreated would have steadily produced spreading paralysis and, potentially, death by asphyxiation. In a state administrative hearing last year, Turner testified, "I tell everybody the story. If I went home per Lakeway Regional's … recommendation, there was a high probability that I would have crashed, and my wife would have been spending the next 25 years wondering what she could have done differently to cause me not to die that night."
Do Right, Risk Consequences
Robert Van Boven saves peoples' lives. He also pisses people off.
The Lakeway neurologist, currently embroiled in a years-long legal combat with the hospital that once employed him, the state agency that attempted to end his career, and a range of lawyers and officials who believe they can wear him down and defeat him, has a long record of getting crossways with the authorities. In one professional position after another, he has consistently refused to go along to get along, and his resistance has cost him dearly. He is described by most fellow professionals as an extraordinarily accomplished doctor – among other distinctions, he was a member of the legendary 1987 Johns Hopkins surgical team that performed a groundbreaking procedure to separate conjoined twins. But he has also repeatedly clashed with institutional expectations, rules, and administrators – and met with recurrent retaliation, most recently severe enough that he fears he may never be able to practice medicine freely again.
A 2014 letter from a former colleague, Lakeway Regional Medical Center hospitalist Dr. Louis Lux, captures a common doubleness of perspectives on Van Boven. "In my 25 years of medical practice in the state of Texas," Lux wrote, "I have never seen a neurologist more dedicated and passionate about patient care and quality of care than Dr. Robert Van Boven. He is among the most intelligent of all neurologists that I have had the pleasure to work beside. … Due to his efforts, care, and concern, many patients have benefited with improved quality of life. At times, some have not understood or fully appreciated the extent of Dr. Van Boven's involvement, and have mistaken his zeal for arrogance or insult. In my experience, nothing could be farther from the truth." Similar statements from other doctors describe Van Boven's selfless dedication to his patients and their welfare, as well as his occasionally contentious personality.
Yet another colleague who now praises him as among the best doctors he has known, and who testified on Van Boven's behalf in an official hearing, also said that Van Boven undoubtedly takes some getting used to. Former LRMC doctor, pulmonary critical care specialist Dr. Raj Babu, described Van Boven's persistence and attention to medical detail: "He was very patient-focused, and he would not stop until … he got what he needed to get for his patient." He recalled the "extreme gratitude of patients and their families" for the level of care Van Boven provided.
Nevertheless, Babu also acknowledged that their initial relationship was "a little rocky." Following their first interactions at LRMC in 2012, he was angered by Van Boven's abrasive manner in a particular instance, and wrote to the hospital's chief administrator, "Frankly, I'm embarrassed to have to work with him at all." Five years later (in a 2017 hearing initiated by the Texas Medical Board), Babu said, "But … coming to understand his approach and coming to understand where that was coming from, and what his ultimate goals were … kind of changed my overall impression of him."
For a reporter working on a complicated, contentious story, Van Boven can be both a godsend and a nuisance – quickly cooperative with any and every inquiry, yet occasionally overwhelming with both excess information and advice. He's both a perfectionist and relentless; were he your neighbor, you wouldn't want him monitoring your lawn maintenance. Yet during a medical emergency, if he happened to become your doctor, he might very well save your life. Both sides of his personality have enabled him to provide critical care for his patients, and to defend fiercely his medical career and professional standing.
For more than a decade, Van Boven has been a serial medical "whistleblower." Recognizing incompetence, negligence, or willful wrongdoing among his institutional superiors or peers, he has refused to look away, and – risking his own livelihood and his family's well-being – has time and again reported what he has found to oversight agencies charged with remediation or discipline. Time and again, his reports of wrongdoing have been confirmed, and he has been vindicated – but only after great personal trouble and cost in money, time, energy, and stress. If he were not so indefatigable and relentless, he would long ago have been broken or ground down into surrender.
Van Boven has consistently confounded the agencies and officials who have fought him or attempted to obstruct him; they have been forced or have chosen to settle the lawsuits he has filed against them. Although, because of these conflicts, he hasn't been able to fully support himself and family through his medical practice alone for several years, the combination of his legal settlement awards and the support of friends and family have thus far sustained him through his ongoing public battles. While still maintaining a reduced practice, he has turned his intellectual talents and seemingly tireless energies to persist in the legal fights that now occupy much of his daily life, in one room of the well-appointed but now only lightly used medical suite he occupies in Lakeway.
"I don't know if I'll ever be able to practice medicine again," he said some months ago. "But I'll be damned if I'm going to let these bastards destroy me."
A selected list of the results of Van Boven's whistleblowing include a 2007 settlement with a Minnesota medical facility over its retaliation against him for reporting hospital harm; a 2010 settlement with the U.S. Department of Veterans Affairs over retaliation for his reports of mismanagement at a VA neurology facility at Pickle Research Campus (Austin); a brief 2010 dismissal from a Defense Department research appointment (reassigned after a public outcry); and most recently (2016-present), an ongoing legal dispute with LRMC and its successor, Baylor Scott & White Medical Center-Lakeway, and the Texas Medical Board, temporary but devastating restrictions on Van Boven's medical practice, and an eventual exoneration last December.
In 2014, following his conflict with the VA that almost ended his career, Van Boven told a U.S. House Committee on Oversight and Government Reform: "Whistleblowers have their roots in stopping crime. They need your protection from persecution and denigration so they can help transparency, integrity, and performance in government today." He added, "I'm going to make this my life passion. … Sam Houston said, 'Do right and risk the consequences.'"
Preventable Errors
Currently, Van Boven (as a co-plaintiff with his private neurology practice, the Brain & Body Health Institute) has lawsuits pending against LRMC and BS&W, and against the Texas Medical Board, the state agency charged with sanctioning doctors for malpractice or other wrongdoing. In the pleadings to those suits, he alleges that the owners and administrators of the hospital retaliated against him because of his internal and external complaints concerning substandard, inadequate, or dangerous care, due to "preventable hospital errors." Many of those complaints (among them one addressing the Marcus Turner case) were subsequently confirmed by regulatory agencies – the Joint Commission (which accredits hospitals), the Centers for Medicare and Medicaid Services, and the Texas Department of State Health Services.
They were not trivial incidents – among the most egregious:
• Failure to properly treat a cardiac staph infection, resulting in a patient's death;
• Inappropriate, unsafe discharge of a patient, contributing to a patient's death;
• Failure to diagnose and treat a severe stroke, "a clear breach in the standard of care";
• Improper treatment of a cardiac arrest and consequent coma, resulting in a patient's death;
• Failure to diagnose and appropriately treat a patient suffering from pneumonia, resulting in a patient's death.
Another representative example: Late one evening in March of 2015, Carolyn Preston called 911 when her husband James began slurring his speech, with facial drooping and weakness on his right side. An ambulance took them to the LRMC emergency room where – despite Carolyn's repeated requests – doctors paid no heed to her fears nor tested for the potential stroke symptoms, instead treating Preston only for high blood sugar. Twelve hours later, a doctor finally responded to Carolyn's complaints, confirmed a stroke diagnosis, and made arrangements for treatment at another hospital – "many hours after the window of time for urgent stroke treatment … had passed." The last phrase is quoted from the Prestons' January 2017 legal pleadings against LRMC and some staff members, in a lawsuit settled late that year.
The Prestons met Van Boven in the wake of that incident, when he reviewed James' medical records and became his doctor. The complaint Van Boven filed (initially with the DSHS) was confirmed as violating the requisite state and federal standards of care, and Van Boven was expecting to testify as an expert witness on James' behalf, when the hospital settled. James credits Van Boven for his recovery ("I still limp a bit in my right leg … it's as good as it's going to get") and for his honesty. "He's a great man," Preston said. "He's out there trying to help people – he's a real doctor."
Bad Faith
Van Boven was hired as the LRMC's sole neurologist when the for-profit hospital opened, in 2012. The Lakeway institution was unusual, in that its $164 million mortgage was guaranteed by the U.S. Department of Housing and Urban Development, in a program intended to address underserved areas. Two years later, the LRMC defaulted on the mortgage, an outcome that would lead (in 2016) to the takeover by Baylor Scott & White.
Van Boven recalls that within a few weeks of his 2012 arrival, he was alarmed by both the lack of necessary medical resources and the low standard of care – other colleagues also noted lack of resources apparently due to cost-cutting – and for the next two years, he made internal complaints of substandard care that he says received little or no effective response. Instead (according to the doctor's subsequent legal filings), his complaints apparently motivated an initial retaliation.
Van Boven learned that in May of 2014 – several months prior to his filing of any complaints to external oversight agencies – an LRMC board member and investor (identified in legal filings as Frank Sossi, then acting chair of the hospital's board of managers) had ignored LRMC's medical peer review committee and independently submitted a file of complaints against Van Boven – edited to exclude exculpatory information – to the Texas Medical Board.
David Kreye, who at the time was LRMC's CEO, subsequently informed the TMB that there was no substance to the complaints, that the hospital's peer review committee had not considered them actionable, and consequently, that the referral to the TMB "may have been made in bad faith." Nevertheless, the TMB explicitly declined to consider the question of bad faith, or of possible administrative retaliation against Van Boven. Instead, the agency initiated its own complaint, and began a three-year pursuit of sanctions against Van Boven.
It had become clear that at least some LRMC owners or administrators had had enough of Van Boven's whistleblowing, and decided he had to go – although how that could be accomplished was yet to be determined. If he refused to leave on his own, other avenues would have to be pursued.
Charges and Threats
Rather than be intimidated, Van Boven fought back, and he no longer felt it necessary to keep his concerns within the hospital. In the fall of 2014, he began to file his complaints with oversight agencies, and over the next year and a half, violations (among them those concerning the Turner and Preston cases) would be confirmed in six separate investigations by staff of the state Department of Health and Human Services, from April of 2015 through of August of 2016.
Simultaneously, TMB legal staff were working their way through the 15 initial complaints filed against the doctor. The TMB would eventually find no violations, nor issue sanctions against Van Boven, but it did offer a "remedial plan" concerning six of the alleged complaints. Van Boven disputed all these findings, and says the TMB prevented him from presenting information in his own defense. In the course of the TMB review, the agency eventually settled on three complaints that would formally result in an "emergency," "temporary" restriction of his practice. That "temporary" sanction would end up lasting nearly two years, greatly undermining Van Boven's work, and effectively devastating his reputation to perhaps the point of no return.
In brief, TMB legal staff identified two female patients (called only "Patient A" and "Patient B" in the official record) who separately accused Van Boven of "boundary violations" – essentially, sexual harassment during appointments at his own medical offices (in April and May of 2015). The patients accused Van Boven of having a visible (downward, within his clothes) erection during part of their initial examinations, and that they believed he may have pressed that erection against their legs while examining their eyes. A third complaint concerned family members of another patient ("Patient C"), who accused the doctor of rude or overbearing behavior.
The three complaints would – after much delay – result first in a "temporary suspension" hearing in February of 2016 (months after they were initially filed), and the consequent imposition of a restriction on Van Boven's medical practice (effective Feb. 29, 2016), forbidding him to treat female patients while he waited for a full hearing. The publication of that "temporary" restriction, and the undeniably salacious charges, severely damaged his medical practice, and he turned much of his considerable energies to his legal actions against the hospital, its owners and managers, and the TMB itself.
Although both state law and the TMB's own rules require due process and an expedited hearing process, it would be late May of 2017 before the matter would be heard before Administrative Law Judge Hunter Burkhalter of the State Office of Administrative Hearings. After a week's hearing and 17 witnesses, including the complainants as well as defense witnesses and Van Boven himself, Burkhalter last September ruled that the TMB staff had failed to prove any of the charges against the doctor.
In a lengthy ruling, Burkhalter described the charges concerning Patient C as essentially baseless, and said there were serious doubts concerning the "accuracy and veracity" of the claims made by Patients A and B. Their testimony (as documented in SOAH transcripts) was inconsistent and contradictory, and might well have been influenced by hospital staff rumor-mongering about Van Boven and (conscious or inadvertent) witness contamination by TMB attorneys. (Moreover, Patient A in her testimony acknowledged demanding $30,000 from the doctor in exchange for her silence.) All three patients or their families, the judge's ruling noted, had various reasons to be upset at Van Boven's diagnoses – and they reacted to those (accurate) diagnoses by blaming the doctor, lending their complaints a taint of retaliation.
Beyond the judge's ruling – technically a "Proposal for Decision," which would finally be confirmed, after even more delay and with great reluctance by the full board in December – there are additional reasons to doubt the independence and fairness of the TMB's actions. Not only had the original action against the doctor been initiated by a non-medical board member with the apparent intention of driving Van Boven out of the hospital, Van Boven had already threatened to sue or sued the hospital for retaliation on three separate occasions, eventually negotiating settlement payments that would total $950,000. One such suit was in progress prior to the Feb. 29, 2016, Temporary Restriction hearing that would result in the limitations on his medical practice. There is evidence that the hospital's legal team may have been aware of the pending hearing and restrictions even before they were made known to Van Boven.
According to the sworn testimony (during the May 2017 SOAH hearing) of Casey Low, one of Van Boven's attorneys, in February of 2016 he'd been trying to schedule a hearing when one of LRMC's attorneys, Thomas Watkins, told him that his clients wanted the doctor to know that if he continued to pursue the lawsuit, "he would never work in this town again." A few days later, Van Boven and his attorney learned of the Temporary Status Restriction Hearing that would result in the long-delayed "emergency" restriction of Van Boven's practice to male patients only. Low testified that he later asked his counterpart if the earlier warning had referred to the TSRH, and Watkins told him yes.
Contacted recently, Watkins said Low's testimony was "not accurate." He said he might have speculated that Van Boven's tendency to sue his employers "might affect his future employability," and that the "male-only" restriction would seem to make a medical practice impossible. "But if the conversation got close to that," Watkins said, "it would have just been me speculating, nothing coming from a client."
If all this were not enough, hospital administrators had gone so far as to attempt to prevent Van Boven from even visiting his patients at the hospital, issuing "no trespass" orders against him. (He had left his LRMC staff position in 2014, establishing his own neurology practice, but retained admitting privileges.) In September of 2016, just after the latest settlement between the LRMC and Van Boven – and a few days after Baylor Scott & White had assumed management of the hospital – Lakeway police officers, encouraged profanely by hospital administrators, arrested Van Boven for violating an already rescinded no-trespass order, in a Keystone Kops-style operation documented on their own body cameras. Van Boven would spend several hours in jail – and sued the officers and the city of Lakeway for false arrest, resulting in a mediated settlement payment to the doctor of $55,000.
Yet Another Whistle
Van Boven has a lawsuit pending against the LRMC investors group and their successors, Baylor Scott & White, as well as a separate action against the TMB, on a range of claims including defamation, civil conspiracy, and retaliation. In addition, the TMB has refused to withdraw the original list of charges filed against him at the National Practitioner Data Bank (a division of the U.S. Department of Health and Human Services), which hospitals and other institutions use for background checks of potential employees. Despite the exoneration ruling by ALJ Burkhalter (and the TMB's own confirmation of that ruling), TMB interim Executive Director Scott Freshour is insisting that the NPDB filing is only "revised," not withdrawn. In a lengthy April 3 letter, the NPDB insisted it has no authority to overrule the TMB's position. (Van Boven believes TMB's refusal to withdraw or "void" the initial filing has already cost him new professional opportunities.)
Moreover, in a remarkable act of vindictiveness, Freshour and the TMB recently retaliated against Judge Burkhalter, complaining to State Office of Administrative Hearings Chief Judge Lesli Ginn that Burkhalter's ruling in the Van Boven case was not only wrong but reflected evidence of bias. Despite Ginn's legal responsibility under state law to protect the "decisional independence" of ALJs, in February Ginn requested and received Burkhalter's resignation "in lieu of termination." That action has resulted in widespread protest inside and outside the agency, further investigations, and calls on Gov. Greg Abbott to end Ginn's tenure. (See "Medical Board Loses a Case … and Attacks the Judge," March 16; and "Uproar Over Judge's Dismissal at SOAH," April 6.)
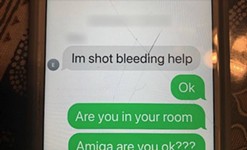
The Van Boven story is not likely to come to an end any time soon. More distressingly, not much appears to have changed at Baylor Scott & White Medical Center-Lakeway, where several of the prior administrators and staff remain in place. On Feb. 20, Van Boven got an evening call from a family friend, Dena McVaney, about her husband Rawney, who earlier that day had gone to the emergency room with weakness in his arms and legs. Five or six hours later, after only cursory examinations and as his condition continued to deteriorate, Rawney was prescribed a sedative, told to go home and rest, and then consult his primary care physician. He left the hospital in a wheelchair – he could no longer walk to the exit door, and when he spoke to Van Boven on the phone that evening, he couldn't lift his arms or move from his couch.
Van Boven rushed to the man's house, quickly confirmed another likely case of Guillain-Barré, and had him transported to Seton Medical Center. He remains in intensive care, with extensive paralysis and receiving assisted breathing via a ventilator. Had Van Boven not intervened, the doctor says, there's a good chance Rawney would not have survived the night.
In late March, Dena told me that her husband's condition remained very serious, and doctors have told her that it might take "six months to a year of convalescent care" for his recuperation. The McVaneys have eight children (two still at home), Rawney is a self-employed commercial broker, and his incapacitation has been "devastating for the whole family." Dena summarized their visit to the Lakeway hospital as several hours of hapless negligence, and said, "If we did not know Robert – I'm not kidding you – Rawney wouldn't be alive." Of Van Boven, she said, "He really does know his stuff, and he is one of those squeaky wheels who gets things done."
On Feb. 27, Van Boven filed another complaint with the state medical oversight authorities (the Department of State Health Services) addressing McVaney's case and his treatment (or lack thereof) at the Lakeway hospital. His report to the DSHS begins in part, "I maintain an acute care hospital facility was in violation of one or more federal and/or state requirements; a failure to diagnose or treat a life-threatening neurological emergency which caused unnecessary delay of time-sensitive treatment and put the patient at peril."
On March 24, a terse, preliminary letter from the Health and Human Services Commission reported: "Based on our investigation, we were able to verify the facility was in violation of one or more federal and/or state requirements. Deficiencies were cited against the facility for violation of the regulatory requirements."
Hero or Martyr?
In various forums, Van Boven has repeatedly denounced what he calls the "culture of silence" concerning failures and inadequacy in U.S. hospital care, citing studies showing that preventable medical errors represent (after heart disease and cancer) the third leading cause of death in the U.S. Citing his own experience, he says that rather than address the problem, too many hospital administrators prefer to ignore it – or worse, suppress attempts to take corrective action. In September of 2014 – prior to the worst of his experiences at Lakeway hospital and the TMB – Van Boven testified to a U.S. House Committee on Oversight and Government Reform about the real consequences of whistleblowing, and what might be done instead to encourage whistleblowers, and defend them from inevitable retaliation.
"I think that the applause for whistleblowing is frustratingly anemic at best," he told the committee. "I think that the current culture is that you have to be masochistic, a Don Quixote, or want to have financial ruin and have a pyrrhic victory and a probable divorce. And these are the statistics. … I myself, thankfully, I survived, but barely.
"So the bottom line," he went on, "is you know we got Boy Scouts and Girl Scouts – you give them badges. We should start early and really make it happen. Where is my badge? I think that if we really want to give positive reinforcements, then make it visible and to say: You are a hero, and mean it. Because right now, people say – oh, they want to applaud a whistleblower, but they don't want to be too close to the whistle."
Dr. Robert Van Boven: A Selected Chronology
1996: M.D., Univ. of Missouri-Kansas City, with related study, research, and practice at Johns Hopkins, Univ. of Maryland, Rush Univ. Medical Center (Chicago), Harvard, and Northwestern Univ.
2000-2003: Clinical Associate, National Institutes of Health (Bethesda, Md.).
2003-2006: Neurologist, Virginia Regional Medical Center (Minnesota); files official complaints concerning substandard care resulting in preventable deaths.
2007: Settles lawsuit against VRMC over violation of a 2005 settlement agreement, defamation and retaliation for justified complaints.
2007-2009: Director of the Brain Imaging and Recovery Lab (J.J. Pickle Center), Dept. of Veterans Affairs; reports prior mismanagement of research funds, is demoted and eventually dismissed; sues VA, claiming retaliation.
2010: VA settles lawsuit, with vindication and payment to Van Boven; confirmation of complaints by U.S. Inspector General.
2009-2012: Dept. of Defense clinical contractor (Fort Riley and Fort Hood).
2012-2014: Neurologist, Lakeway Regional Medical Center. Files internal complaints concerning "medical errors, lack of resources … and competency of hospital staff."
2014: Van Boven leaves hospital staff (opening own neurology practice), retains admitting privileges.
May, 2014: LRMC board member, ignoring medical peer reviews and redacting exculpatory materials, files complaints against Van Boven with Texas Medical Board.
Sept. 2014: First of three eventual settlements with LRMC of Van Boven claims charging retaliation; over time, LRMC will pay $950,000 in mediated settlements for retaliation and defamation; Van Boven testifies before congressional committee about his VA experience and the consequences of whistleblowing.
2014 (fall)-2016: Van Boven begins filing medical care complaints against LRMC to regulatory authorities; violations confirmed in six separate investigations by Texas Dept. of Health and Human Services; TMB begins investigation of Van Boven.
Feb. 29, 2016: TMB imposes "emergency," "temporary" restriction on Van Boven's practice to male patients only (nine months after two patient allegations of "boundary violations").
Sept. 1, 2016: Baylor Scott & White assumes management of LRMC, becoming Baylor Scott & White Medical Center-Lakeway.
Sept. 7, 2016: Van Boven arrested for trespass at hospital while attempting to visit patient; city of Lakeway subsequently pays mediated settlement for false arrest.
May 2017: Five-day hearing of TMB charges against Van Boven before State Office of Administrative Hearings.
Sept. 15, 2017: SOAH Administrative Law Judge Hunter Burkhalter issues "Proposal for Decision" exonerating Van Boven of all TMB charges; in December, TMB reluctantly confirms Burkhalter's PFD.
Jan. 10, 2018: TMB Exec. Dir. Scott Freshour writes letter of complaint to SOAH concerning Judge Burkhalter.
Feb. 22, 2018: SOAH Chief ALJ Lesli Ginn accepts Burkhalter's resignation "in lieu of termination."
March 24, 2018: State Health and Human Services Commission confirms "federal and/or state" violations at Baylor Scott & White Medical Center-Lakeway, concerning failure to treat emergency patient Rawney McVaney on Feb. 20, as reported by Van Boven; McVaney remains in intensive care.
Got something to say on the subject? Send a letter to the editor.